Overview
The ruptured Abdominal Aortic Aneurysm is a medical emergency which is often fatal. The classic triad of “shock, abdominal pain and a pulsatile mass” is not always present and the urgency of the situation not therefore recognised1. It is suggested that a misdiagnosis rate for ruptured Aortic Aneurysms may be as high as 42% with incorrect diagnosis including renal colic (6%), myocardial infarction (6%), colonic inflammation (3%) and gastrointestinal perforation (3%).
This issue persists and has not been improved by better diagnostics and surgical imaging. As the frequency of Aortic Aneurysms and their acute rupture diminish with screening and falling cardiovascular disease rates the diagnostic challenge for a rare event will become harder.
Signs and Symptoms
The ruptured Abdominal Aortic Aneurysm is a medical emergency which is often fatal. The classic triad of “shock, abdominal pain and a pulsatile mass” is not always present and the urgency of the situation not therefore recognised1. It is suggested that a misdiagnosis rate for ruptured Aortic Aneurysms may be as high as 42% with incorrect diagnosis including renal colic (6%), myocardial infarction (6%), colonic inflammation (3%) and gastrointestinal perforation (3%).
This issue persists and has not been improved by better diagnostics and surgical imaging. As the frequency of Aortic Aneurysms and their acute rupture diminish with screening and falling cardiovascular disease rates the diagnostic challenge for a rare event will become harder.
Signs and Symptoms
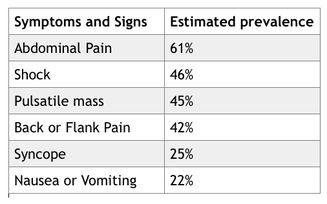
The rupture of an aortic aneurysm may occur abruptly and catastrophically or can evolve over a few hours or days as the leak is tamponaded by surrounding tissues.
The symptoms that occur depend upon the location of the bleeding, with ~80% of ruptures being retroperitonieal2.
The conditions prevalence increases with age over 55, smoking and hypertensive history with males developing the condition 10 years earlier than women3,4 Clearly if the patient is known in advance of symptoms to have an enlarged aorta then raising concern regarding a possible diagnosis in the presence of back or abdominal pain is somewhat easier.
The rare and unusual presentations can include
Actions
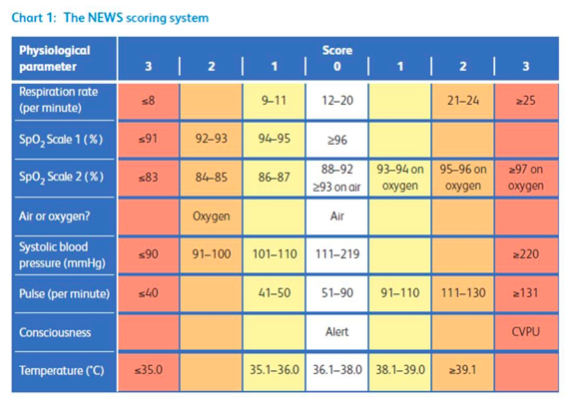
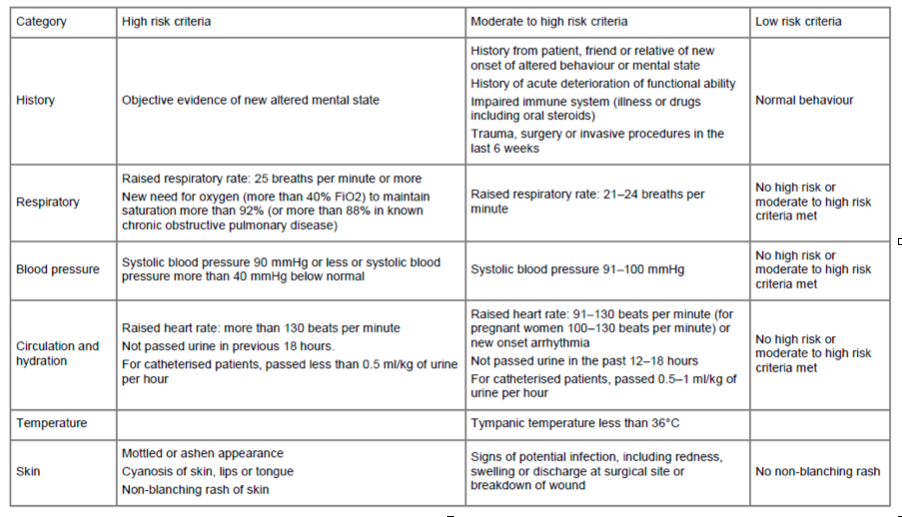
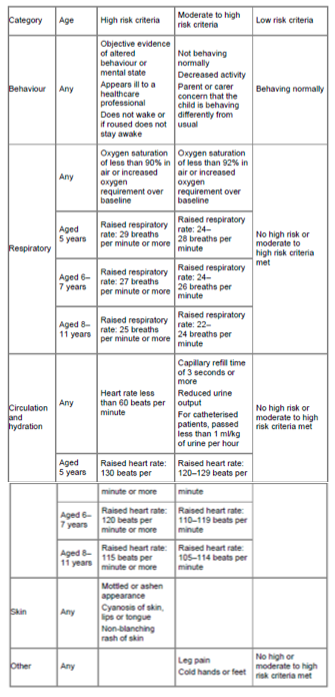
Ruptured aortic aneurysm should not be discounted from the differential diagnosis of sudden back or abdominal pain, because hypotension or a pulsatile mass are absent. Consideration should be given to taking physical observations and calculating a NEWS score where there is diagnostic uncertainty. Awareness of some of the other features which may present is likely to be helpful.
Summary
1. Azhar B, Patel SR, Holt PJE, Hinchliffe RJ, Thompson MM, Karthikesalingam A. Misdiagnosis of Ruptured Abdominal Aortic Aneurysm: Systematic Review and Meta-Analysis. Journal of Endovascular Therapy 2014; 21(4): 568-75.
2. Assar AN, Zarins CK. Ruptured abdominal aortic aneurysm: a surgical emergency with many clinical presentations. Postgrad Med J 2009; 85(1003): 268-73.
3. Reite A, Soreide K, Ellingsen CL, Kvaloy JT, Vetrhus M. Epidemiology of ruptured abdominal aortic aneurysms in a well-defined Norwegian population with trends in incidence, intervention rate, and mortality. Journal of vascular surgery 2015; 61(5): 1168-74.
4. Aggarwal S, Qamar A, Sharma V, Sharma A. Abdominal aortic aneurysm: A comprehensive review. Experimental and clinical cardiology 2011; 16(1): 11-5.
Download the PDF.
The rare and unusual presentations can include
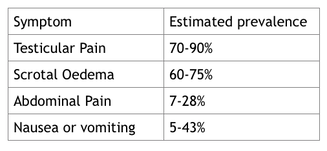
- Transient lower limb paralysis
- Right hypochondrial pain
- Nephroureterolithiasis
- Groin pain
- Testicular pain
- Testicular ecchymosis (blue scrotum sign of Bryant)
- Iliofemoral venous thrombosis
- Inguinoscrotal mass mimicking a hernia
Actions
Ruptured aortic aneurysm should not be discounted from the differential diagnosis of sudden back or abdominal pain, because hypotension or a pulsatile mass are absent. Consideration should be given to taking physical observations and calculating a NEWS score where there is diagnostic uncertainty. Awareness of some of the other features which may present is likely to be helpful.
Summary
- Ruptured aortic aneurysm is a fatal surgical emergency
- The classic triad of pain, hypotension and a pulsatile mass is present in only 25-50% of patients
- Different sites of aneurysm rupture determine the various clinical presentations seen in patients
- Early recognition of these presentations and prompt treatment of ruptured aneurysms is life saving
1. Azhar B, Patel SR, Holt PJE, Hinchliffe RJ, Thompson MM, Karthikesalingam A. Misdiagnosis of Ruptured Abdominal Aortic Aneurysm: Systematic Review and Meta-Analysis. Journal of Endovascular Therapy 2014; 21(4): 568-75.
2. Assar AN, Zarins CK. Ruptured abdominal aortic aneurysm: a surgical emergency with many clinical presentations. Postgrad Med J 2009; 85(1003): 268-73.
3. Reite A, Soreide K, Ellingsen CL, Kvaloy JT, Vetrhus M. Epidemiology of ruptured abdominal aortic aneurysms in a well-defined Norwegian population with trends in incidence, intervention rate, and mortality. Journal of vascular surgery 2015; 61(5): 1168-74.
4. Aggarwal S, Qamar A, Sharma V, Sharma A. Abdominal aortic aneurysm: A comprehensive review. Experimental and clinical cardiology 2011; 16(1): 11-5.
Download the PDF.

 RSS Feed
RSS Feed
